Абстракт
Поздняя стадия рака молочной железы требует комплексного, мультидисциплинарного подхода, включающего как хирургическое вмешательство, так и реконструктивные методы лечения. Модифицированная радикальная мастэктомия, применяемая для локального контроля опухоли, может негативно повлиять на самооценку и психоэмоциональное состояние пациентки. В настоящем клиническом случае описывается поэтапная аутологичная реконструкция у 44-летней пациентки, диагностированной с инвазивной протоковой карциномой, обширным кожным поражением и метастазами в костную ткань. Первая попытка реконструкции с использованием расщеплённого кожного трансплантата оказалась неудачной вследствие некроза трансплантата. На втором этапе был применён миокутанный лоскут на широчайшей мышце спины, что позволило достичь положительного результата и обеспечить своевременное продолжение адъювантной терапии. Данный случай подчёркивает важность индивидуализированных хирургических стратегий и слаженного мультидисциплинарного взаимодействия при реконструкции дефектов, возникающих в ходе лечения рака молочной железы на поздней стадии. Аутологичные методы, особенно у пациенток, проходящих лучевую терапию, способствуют улучшению заживления, снижению частоты осложнений и повышению как функциональных, так и онкологических показателей.
Сопроводительное письмо
Introduction
Breast cancer is among the most prevalent malignancies affecting women globally, necessitating comprehensive treatment plans—especially in advanced stages (Bray et al., 2018). One of the most widely adopted surgical approaches for achieving local tumor control in such cases is the modified radical mastectomy (MRM). However, MRM often results in the loss of one or both breasts, which can contribute significantly to physical discomfort and psychosocial distress (Al-Ghazal et al., 2000; Pusic et al., 2007).To mitigate these negative effects, reconstructive surgery has become an essential part of post-mastectomy care.
Several studies have highlighted its benefits in enhancing quality of life and restoring body image, particularly in younger or advanced-stage patients (Pusic et al., 2007). In patients who are expected to undergo radiotherapy or chemotherapy, progressive reconstruction techniques are favored. These methods allow flexibility in staging the reconstructive process to accommodate the effects of adjuvant therapies (Kronowitz & Mandujano, 2015).Autologous reconstruction especially using TRAM, DIEP, or latissimus dorsi flaps has been widely adopted for its durability and compatibility with radiation therapy (Manrique et al., 2019). In particular, delayed or staged reconstructions are strongly recommended for patients undergoing post-mastectomy radiotherapy, as they reduce the risk of postoperative complications and improve aesthetic results (Berry et al., 2010).In this case report, we present a patient with locally advanced breast cancer who underwent a staged autologous breast reconstruction. The report evaluates clinical outcomes, complication profile, and patient satisfaction, while referencing evidence-based approaches from the current literature.
Case Presentation
A 44-year-old female patient presented with a firm, immobile mass located near the areolar region of the right breast. The lesion measured approximately 3 cm in diameter. The patient reported no significant personal or family history of malignancy.Breast ultrasonography revealed a suspicious 26 × 17 mm lesion at the 10–12 o’clock position, accompanied by skin thickening and nipple retraction.
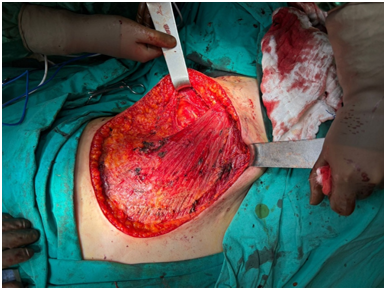
The lesion was categorized as BI-RADS 5, and an axillary lymph node measuring 30 mm with cortical thickening of 8 mm was also detected. Under ultrasound guidance, tru-cut biopsies were performed on both the primary mass and the axillary lymph node.Histopathological examination confirmed invasive ductal carcinoma in the right breast. Immunohistochemical markers showed ER positivity at 30%, PR positivity at 50%, HER2 negativity, and a Ki-67 index of 20%. The axillary node was also confirmed as metastatic. Staging with PET-CT revealed bone metastases involving the sternum and L3 vertebra, with SUVmax values of 4.3 for the primary lesion, 3.8 for the lymph node, and 3.7 for metastatic bone foci.The case was presented at a multidisciplinary tumor board, which recommended systemic therapy with Letrozole, Ribociclib, Denosumab, and Goserelin. Despite initial medical management, the breast lesion progressed. Re-evaluation by the tumor board resulted in a surgical plan targeting the primary lesion. Preoperative physical examination demonstrated extensive skin involvement affecting all quadrants of the right breast, including the nipple-areola complex (Figure 1). MRI confirmed the absence of chest wall invasion. Given the skin infiltration, a wide local excision involving the entire breast skin was planned.A right modified radical mastectomy was performed with the collaboration of general and plastic surgery teams. In the same session, a split-thickness skin graft was used for immediate reconstruction (Figure 2).However, by the first postoperative week, signs of ischemia appeared in the graft (Figure 3), which evolved into full-thickness necrosis in subsequent days (Figure 4). Final pathology showed that 25 of 32 axillary lymph nodes were metastatic, and the tumor extended to the pectoral muscle. Due to the failure of the skin graft, a second-stage reconstruction was performed using a latissimus dorsi myocutaneous flap, known for its vascular reliability (Figure 5).
The patient recovered uneventfully from this procedure and was referred for adjuvant radiotherapy and systemic therapy.Written informed consent was obtained from the patient for publication of clinical details and images.
Discussion
Breast reconstruction following modified radical mastectomy (MRM) in advanced-stage breast cancer requires careful multidisciplinary planning, balancing oncological safety with reconstructive success. In this case, tumor progression despite systemic treatment and the presence of bone metastasis necessitated a wide surgical excision, which directly influenced the choice of reconstruction method.The initial use of a split-thickness skin graft, selected for immediate reconstruction, was likely compromised by the patient’s systemic therapy. The development of ischemia and necrosis in the graft ( Figures 3 and 4) underscores the detrimental impact of chemotherapy on wound healing, particularly in aggressive malignancies ( Berry et al., 2010).Several studies have reported that implant-based reconstructions carry an increased risk of complications such as capsular contracture, infection, and implant loss when performed in patients receiving post-mastectomy radiotherapy (Ho et al., 2012). In contrast, autologous tissue reconstructions, especially those using well-vascularized flaps, are more resilient to radiation-related damage and are therefore preferred in high-risk or radiotherapy-bound patients (Kronowitz & Mandujano, 2015).In the current case, the latissimus dorsi myocutaneous flap (LDMF) was selected for the second-stage reconstruction. This flap is known for its consistent vascularity and adequate tissue volume, making it particularly suitable for covering large post-mastectomy defects (Chang et al., 2012).
As shown in Figure 5, the flap resulted in successful healing and volume restoration, even in an irradiated and surgically traumatized field. Another key advantage of this staged, autologous approach was the uninterrupted continuation of adjuvant therapies, which is critical for patients with advanced disease (Schaverien et al., 2018). The patient in this case was able to proceed with both radiotherapy and systemic chemotherapy without delay, reflecting one of the major clinical benefits of choosing staged autologous reconstruction. Beyond surgical outcomes, patient-centered goals such as body image, sexual well-being, and overall quality of life are significantly improved through breast reconstruction. Instruments like the BREAST-Q, which evaluate patient-reported outcomes, have consistently shown higher satisfaction rates in reconstructed patients compared to those who undergo mastectomy alone (Pusic et al., 2009; Eltahir et al., 2013). Nevertheless, the cumulative burden of advanced cancer and its treatments must be taken into account when evaluating long-term psychosocial benefits.This case thus reinforces the value of personalized and flexible reconstruction planning. It also highlights how multidisciplinary coordination between surgical oncology, plastic surgery, and radiation oncology can reduce morbidity, accommodate oncological requirements, and ultimately improve patient satisfaction and recovery.
Conclusion:
In patients requiring radiotherapy, autologous tissue reconstruction offers a dependable solution due to its ability to withstand radiation effects and promote proper healing. This case underscores the importance of a collaborative, multidisciplinary approach that integrates oncologic and reconstructive expertise. Tailoring surgical strategies to individual patient conditions, especially in complex or advanced-stage scenarios, is essential for minimizing complications, maintaining treatment continuity, and enhancing overall outcomes. The success of a staged, flexible approach highlights the value of adapting reconstruction plans in real-time to meet evolving clinical needs.
Фигуры

Ключевые слова
Ссылки
1. Al-Ghazal, S. K., Fallowfield, L., & Blamey, R. W. (2000). "Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy, and breast reconstruction." European Journal of Cancer, 36(15), 1938-1943.
2. Berry, T., Brooks, S., Sydow, N., et al. (2010). "Complication rates of radiation on tissue expander and autologous tissue breast reconstruction." Annals of Surgical Oncology, 17(3), 202-210.
3. Bray, F., Ferlay, J., Soerjomataram, I., et al. (2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries." CA: A Cancer Journal for Clinicians, 68(6), 394-424.
4. Kronowitz, S. J., & Mandujano, C. C. (2015). "Delayed-immediate breast reconstruction: Technical and timing considerations." Plastic and Reconstructive Surgery, 136(2), 283-293.
5. Manrique, O. J., Kapoor, T., Banuelos, J., et al. (2019). "Single-stage direct-to-implant breast reconstruction: A comparison between submuscular and prepectoral implant placement." Plastic and Reconstructive Surgery, 144(5), 1077-1084.
6. Pusic, A. L., Klassen, A. F., Scott, A. M., et al. (2007). "Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q." Plastic and Reconstructive Surgery, 120(2), 345-353.
7. Chang, D. W., Youssef, A., Cha, S., et al. (2012). "Autologous breast reconstruction with the extended latissimus dorsi flap." Plastic and Reconstructive Surgery, 130(4), 751-761.
8. Eltahir, Y., Werners, L. L., Dreise, M. M., et al. (2013). "Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures." Plastic and Reconstructive Surgery, 132(2), 201e-209e.
9. Ho, A. L., Bovill, E. S., Macadam, S. A., et al. (2012). "Postmastectomy radiation therapy after immediate two-stage tissue expander/implant breast reconstruction: a University of British Columbia perspective." Plastic and Reconstructive Surgery, 130(1), 1e-10e.
10. Pusic, A. L., Matros, E., Fine, N., et al. (2009). "Patient-reported outcomes 1 year after immediate breast reconstruction: results of the Mastectomy Reconstruction Outcomes Consortium Study." Journal of Clinical Oncology, 35(22), 2499-2506.
11. Schaverien, M. V., Macmillan, R. D., & McCulley, S. J. (2018). "Is immediate autologous breast reconstruction with postoperative radiotherapy good practice?: a systematic review of the literature." Journal of Plastic, Reconstructive & Aesthetic Surgery, 66(12), 1637-1651.
О статье:
История публикации
Опубликовано: 30.Apr.2025
Авторское право
© 2022-2025. Azerbaijan Medical University. E-Journal is published by "Uptodate in Medicine" health sciences publishing. All rights reserved.Связанные статьи
ХРОНИЧЕСКАЯ ГИПОКСИЯ И ИММУНОПАТОЛОГИЧЕСКИЙ ПРОФИЛЬ ПРИ ВРОЖДЁННЫХ ПОРОКАХ СЕРДЦА У ДЕТЕЙ
Просмотрено: 993



